by John A. Baur, PT, DPT, OCS, CSCS, FAAOMPT
Can individuals return to sports after ACL injury without reconstruction? And, who needs surgery?

Typical pre-op rehabilitation goals include:
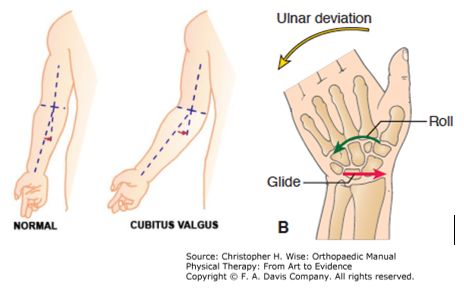
No pre-operative flexion contracture or quadriceps lag
– Quad contraction with superior glide of the patella
– Normal patellar mobility
Little to no effusion (swelling within the knee joint space)
Walk without a limp
What are successful outcomes?
Lynch BJSM 2015
A survey was performed on almost 2000 orthopedic surgeons, and sports/rehabilitation specialists in Europe. These specialists across-the-board only had two things that came up from virtually everybody about what successful outcomes equal success.
1) Return to sports or previous activity
Moon cohort data football in the United States found that 63% of American Football player (AFB) and 69% of high school football players (HS FB) of the players were able to return to play at the same self-described performance level. Approximately 27% felt they did not perform at the level attained before their ACL injury/tear, and 30% were unable to return to play at all.
The Moon cohort data for soccer in the United States found that 72% of soccer players returned to play.
Clare Ardern, Australian-trained physiotherapist and senior researcher in sports medicine, performed a meta-analysis in 2011 found that 63% of athletes returned to preinjury level of spots and 44% to competitive sports. This is the same results found in the Moon cohort.
Shah et al AJSM 2010 published that in NFL players underwent ACL reconstructions 61% (31/49) returned to playing in the NFL at a mean of 11 months after surgery.
Feucht et al 2014 conducted a survey of what patients think prior to undergoing ACL reconstructive surgery. The study found that 94% of primary or initial ACL reconstruction and 84% of revised ACL reconstruction expect to return to the same level of activity with no or slight restrictions. The patients’ preoperative expectations do not match the post-operative outcome data.
2) No reinjury (Does this really happen)?
– Moon cohort data found that 20% of women soccer players suffer ACL reinjury.
– Paterno et al (Hewett prevention cohort) 20% in the those 18 and younger sustained an ACL reinjury.
– Shelbourne data set showed that 17% in college age athletes and younger endured an ACL reinjury.
– Pinczewski data set revealed that ACL reinjury was 17% higher in younger athletes and in males.
– All rates were higher with allografts (tissue that is transplanted from one person to another) in younger athletes.
Contralateral, or opposite side, ACL reinjury is 12-25% higher in younger athletes and females.
Osteoarthritis was seen in 45-70% patients 15 years after ACL reconstructive surgery and higher in those who returned to strenuous sports. However, if you ask patients what they think their risk of developing osteoarthritis will be 98% will say “they have no or slight increased risk”.
After ACL revision surgery
– Patient have a worse outcome in the short-term
– Higher occurrence of osteoarthritis and higher degree of disability in the long-term.
In a study conducted by Paterno et al AJSM 2014, they followed post- ACL reconstruction patients and a control group (teammates) of the athletes who played sports that require cutting, pivoting or jumping movements for 24 months.
The study found that 29.5% of the athletes with a history of ACL reconstruction suffered a second ACL injury while only 8.5% of the control athletes suffered a first ACL injury.
The overall incidence rate of a second ACL injury was nearly 6 times greater than the control subjects in the 24-month period.
Within the ACL reconstruction group, female athletes were more than twice as likely to tear the ACL on their contralateral (opposite side) knees rather than the graft in the surgical knee.
Athletes in the ACL reconstruction group who suffered another ACL injury did so soon after they returned to play. 30.4% were injured in less than 20 athletes-exposures, and 52.2% were injured in less than 72 athletes-exposures.
In a meta-analysis conducted by Webster et al AJSM 2014 found that in patients younger than 20 years of age at the time of surgery, 29% sustained a subsequent ACL injury to either knee. The odds for sustaining an ACL graft rupture or contralateral injury increased 6- and 3-fold, respectively, for patient younger than 20 years.
Returning to cutting/pivoting sports increased the odds of graft rupture by a factor of 3.9 and contralateral rupture by a factor of 5. Also, a positive family history doubled the odds for both graft rupture and contralateral ACL injury.
In a study conducted by Wiggins et al AJSM 2016 found that secondary ACL injury rate (ipsilateral and contralateral) for patients younger than 25 years was 21%. The secondary ACL injury rate for athletes who return to a sport was also 20%. Combining these risk factors, athletes younger than 25 years who return to cutting, pivoting or jumping sport have a secondary ACL injury rate of 30%.
Are orthopedic surgeons and physical therapist appropriately counseling patients regarding ACL reconstructive surgery?
Patients see the successful ACL reconstructive surgery outcome on TV and social media.
What should orthopedic surgeons and physical therapist be counseling patients regarding ACL reconstructive surgery?
– Just because you have an ACL reconstruction, doesn’t mean that you will return to sport at all, and most likely not at the same level of performance.
– Your risk of reinjury is high in the near term or short after returning to play, reinjury is higher if you are younger, higher (ipsilateral or same side) if you are male and (contralateral or opposite side) if you are female.
– Regardless of the type of ACL reconstruction surgery, your risk of developing osteoarthritis is high in the long-term and if you need a revision of the ACL reconstruction surgery the risk of osteoarthritis is higher.
At Physical Therapy First we believe that providing true sport physical therapy requires a physical therapist who is “evidence informed and clinically astute”. Physical Therapy First works hard to stay well-informed with the best and latest true sports physical therapy research and our residency / fellowship trained physical therapist are clinically skilled and astute. We believe this makes a true difference in our patient physical outcomes and successful return to sports.
References:
Shah VM, Andrews JR, Fleisig GS, McMichael CS, Lemak LJ. Return to play after anterior cruciate ligament reconstruction in National Football League athletes. Am J Sports Med. 2010 Nov; 38 (11): 2233-9.
Kaeding CC, Pedroza AD, Reinke, EK, Laura J. Huston, LJ, MOON Consortium, and Spindler, KP. Risk Factors and Predictors of Subsequent ACL Injury in either Knee after ACL Reconstruction: Prospective Analysis of 2488 Primary ACL Reconstructions from the MOON Cohort. Am J Sports Med. 2015 Jul; 43(7): 1583–1590.
Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med, 2011.
Feucht MJ, Cotic M, Saier T, Minzlaff P, Plath JE, Imhoff AB, Hinterwimmer S. Patient expectations of primary and revision anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016 Jan;24(1):201-7. doi: 10.1007/s00167-014-3364-z. Epub 2014 Oct 2.
Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567–1573.
Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(3):641–647.
Wiggins Amelia, Grandhi Ravi, Schneider Daniel, Stanfield Denver, Webster Kate, Myer Gregory. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: A systematic review and meta-analysis Am J. Sports Med. 2016 July; 44(&): 1861-1876
Lynch A D, Logerstedt D S, Grindem H, Eitzen I, Hicks G E, Axe M J, Engebretsen L, Risberg M A, Snyder-Mackler L. Consensus criteria for defining ‘successful outcome’ after ACL injury and reconstruction: a Delaware-Oslo ACL cohort investigation. British Journal of Sports Medicine Mar 2015, 49 (5) 335-342.
NSMC (June 2016) Lynn Snyder-Mackler – Is there a place for non-operative treatment for ACL tears presentation.