Concussions and Post Concussion Syndrome
By Lillian Byington PT, DPT, OCS, CMPT
Up to 3 million people each year seek medical treatment for concussions and concussion related symptoms; and further research indicates that up to half of people experiencing concussion do not report their symptoms. This suggests that up to 6 million people each year experience symptoms of concussion. While most people recover within a few weeks, 14-33% of patients complain of persistent symptoms 3+ months after injury. Current testing for concussion is limited. In the first 3 days after injury, there are some standardized assessments such as bloodwork, CT, and/or MRI which can be performed to diagnose concussion. These are often impractical and are not yet commonly used in the diagnosis or treatment of concussion.[/caption]
While most people recover within a few weeks, 14-33% of patients complain of persistent symptoms 3+ months after injury. Current testing for concussion is limited. In the first 3 days after injury, there are some standardized assessments such as bloodwork, CT, and/or MRI which can be performed to diagnose concussion. These are often impractical and are not yet commonly used in the diagnosis or treatment of concussion.[/caption]
Once 4-5 days after injury have passed, there are no specific tests for concussion. Becoming more common is the use of physical therapy to treat the symptoms associated with concussions to maximize return to sport. Below we have summarized the most common symptoms and reviewed what physical therapy treatment addresses in order to treat patients.
● Dizziness
60% of people suffering from concussion complain of dizziness. Physical therapy exam consists of testing your vision, how well you can track moving objects, balance, and inner ear function. Once we know which aspects are contributing to symptoms of dizziness, we can design a treatment program to help address any deficits you may have
● Memory loss and/or exercise intolerance
Memory loss and exercise intolerance seem to be correlated in patients after concussion. Research suggests that this is due to cerebral blood flow changes in the first 3 days after injury. While these symptoms can persist for weeks to months, blood flow changes seem to resolve within the first 3 days. We use a combination of endurance/cardiovascular tests and patient reported symptoms to design a gradual exercise program to minimize these symptoms
● Visual disturbances
42-55% of patients note visual disturbances after concussion. A full exam to test your vision and how well you track moving objects can help differentiate these symptoms from dizziness. Once we know which aspects are contributing to your symptoms, we can design a treatment program to help address any deficits you may have
● Mood changes/anxiety
25% of patients with concussion report new symptoms of anxiety and mood changes. These are usually assessed with patient history and subjective reports
● Migraine headache
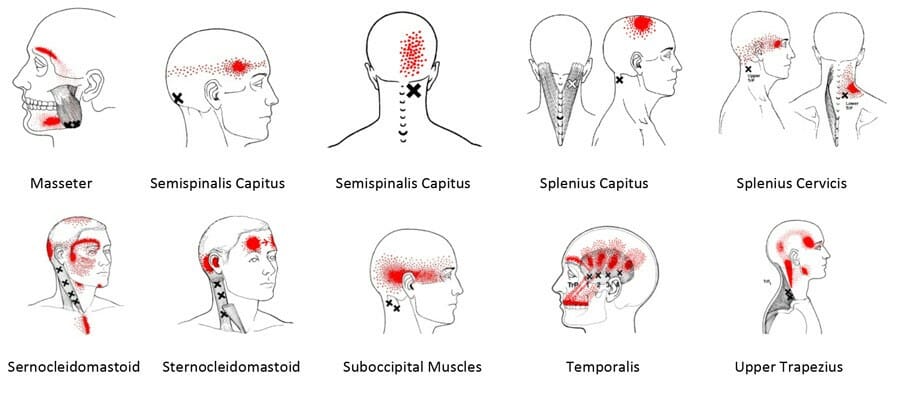
70% of patients with concussion report new onset of migraine headaches. There is an international classification criteria to diagnose migraine vs headache. A full exam of your neck will also help us determine what is causing your headaches. Once we know what your deficits are, we can coordinate with your doctor and/or treat any physical impairments we have found in order to reduce your headache.
● Neck pain
Neck pain can also contribute to headaches and dizziness. A full neck exam, visual exam, and balance screen can help us determine what specifically is causing your symptoms and allow us to design a treatment plan to address your specific issues to help you feel better
● Cognitive deficits
Changes in mental function are some of the first diagnosis tools we had for concussion. Studies suggest these deficits can last days to months. While pre-injury baseline testing is useful, it is not necessary. We use a combination of patient history and dynamic balance/memory tests to help determine what your deficits are and incorporate them into your treatment plan
Recovery from concussions
Clinical recovery from a concussion (what the patient reports as their symptoms) is often very different from physiological recovery from concussion. We know changes in electrical response, metabolic balance, and oxygen consumption persist for several months after a patient’s clinical testing comes back normal and patients report being symptom free. We base most of our return to activity on the clinical tests listed above, and patient reports of symptoms.
Allowing clinical signs to completely resolve before returning to sport not only reduces the risk for future concussion, but also reduces the risk of other injury.
What does this mean for me?
If you have been diagnosed with a concussion OR if you feel that you may have suffered a concussion, and are still dealing with side effects, physical therapy can help. Here at PT First we focus on what your symptoms are and how they affect you, and use that to guide our examination and treatment plan so we can get you back to your activities.
Original Article – Diagnosis and Management of Concussion
Mucha, Anne, and Alicia Trbovich. “Considerations for Diagnosis and Management of Concussion.” Journal of Orhopaedic and Sports Physical Therapy, vol. 49, ser. 11, Nov. 2019, pp. 787–798. 11.