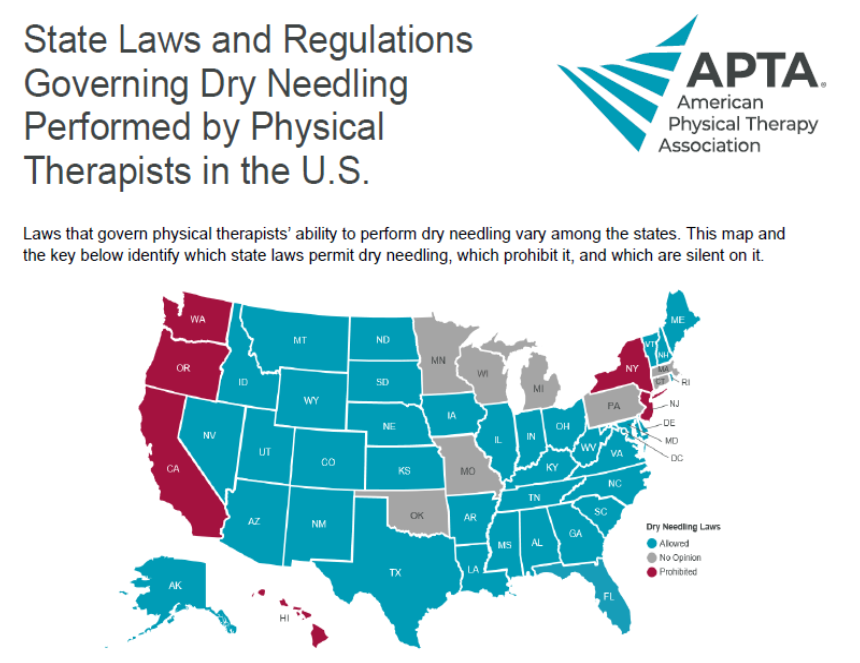
Exercises to Help Improve Weight Acceptance and Standing Tolerance on the Lower Extremity Following Injury or Surgical Procedure
Following an injury or surgical procedure to the hip, knee, or ankle it is often painful and difficult to put weight through the affected leg. Often times, we avoid putting weight through the affected leg due to a large amount of pain and use an assistive device such as a walker or cane to help us offload our weight using our arms. Using an assistive device and limiting weight through the affected leg is beneficial early on, especially for those with weightbearing restrictions, to help promote proper healing. However, when ready and able to, it is good to start practicing putting more weight through the affected limb as early as possible to help your body get used to these stresses. When doing this, please consider your pain and swelling levels as both serve as a great guide to determine the amount one should perform. Also, please take into account your safety and consider practicing weight acceptance exercises with an assistive device or something sturdy nearby to hold onto.
Here is a progression of some common, simple exercises to help improve weight acceptance and standing tolerance for an affected lower extremity. These are great exercises one can perform at home as part of their home exercise program, however discuss proper technique and dosage with your physical therapist before performing independently.
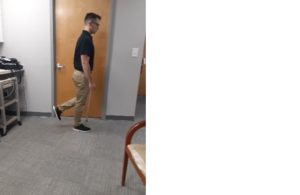
In each picture, my RIGHT leg is the affected side and I am using a cane with my LEFT hand or holding on to a sturdy chair to help offload and balance.
| Lateral Weight Shifts: Start standing with equal weight distribution and shift body weight onto affected leg.
|
 |
| Forward Weight Shifts: Start standing with most body weight on non-affected leg with affected leg in front, shift body weight onto affected leg. |  |
| Lateral Weight Shifts onto Single Leg Stance with Holding On: Shift body weight onto affected side with picking up foot of non-affected leg off the ground while holding on with hands for support. |  |
| Forward Weight Shifts onto Single Leg Stance with Holding On: Shift body weight onto affected side with picking up foot of non-affected leg off the ground while holding on with hands for support
|
 |
| Lateral Weight Shifts onto Single Leg Stance without Holding On: Shift body weight onto affected side with picking up foot of non-affected leg off the ground and do not hold on to accept 100% of body weight.
|
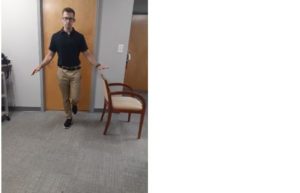 |
| Forward Weight Shifts onto Single Leg Stance without Holding On: Shift body weight onto affected side with picking up foot of non-affected leg off the ground and do not hold on to accept 100% of body weight.
|
 |
| Single Leg Stance with Opposite Lower Extremity Movements: Great exercise to work on standing tolerance and hip stability. Feel free to perform with or without holding onto a sturdy object depending on the recommendation from your PT.
3 way hip – while standing on the affected limb, move your other leg out in front of you, out to the side, and behind you.
Circles – while standing on the affected limb, move your other leg in small circles in a clockwise and counterclockwise directions. |
   |
These exercises above are some of the more common ones I like to prescribe to patients, however there are multiple other variations to challenge our bodies in different ways. Weight acceptance exercises are only one part of a comprehensive physical therapy routine that may benefit you following injury or surgery to a lower extremity. The physical therapists at Physical Therapy First assess each patient on an individual level and determine PT interventions specific to each person’s needs. We spend 1 on 1 time with our patients for a full hour for every PT session.