by ptfadmin | Dec 14, 2022 | Health Tips
Written by Mark Boyland PT, DPT, CSCS
What if I told you there was a non pharmaceutical way to promote pain relief or maybe more accurately a way to reduce your perception of pain through exercise? What if you could continue moving and exercising your other non painful body parts and that the exercise would benefit your painful body parts? What if it only took 15 minutes of aerobic exercise where your heart rate reached at least 120? Would you take that option? Let’s explore more.
This study explored patient’s pain perception levels before and after a bout of aerobic exercise. The study design included 20 females and 10 males who averaged 20.6 years old. The researchers made sure that the participants had no history of shoulder pain prior to performing the study. The researchers used an algometer, a device that applies pressure and measures the pounds/cm2 applied until there is a report of pain. The researchers performed this measure 4 times in total. Twice in the first day with 15 minutes between measurements and then again 24-48 hours later with the third test being prior to performing aerobic exercise and the fourth and final test after aerobic exercise. The researches chose a NuStep for the aerobic exercise and told participants to only use their legs to perform the exercise bout.
As an average the participants had relatively similar algometer readings at measures 1,2,and 3 with an increase in tolerance for the 4th measure after aerobic exercise of approximately 1.5-1.9 pounds/cm2. Of note however, the females had a more consistent baseline measure at 11.4, 11.0, and 11.9 with a 4th measure of 13.6 whereas the male participants had decreasing readings with a generally increased 4th reading at 17.3, 16.5, 15.6, and 17.4.
The evidence may not be very strong for the use of aerobic exercise of non painful extremities to reduce pain in painful extremities however there may be some merit. Regardless, continuing with a form of tolerable and preferred aerobic exercise is still recommended for general health and wellness regardless of the presence of pain. Additional studies are needed with larger sample sizes and possibly to include participants who have shoulder pain as opposed to recreating shoulder pain with a tool. Regardless, as a physical therapist if I can provide my patients with a non pharmacological and non modality based pain relief who am I to deny them?
Do you think it’s worth 15 minutes of your time?
PMCID: PMC7015025
by ptfadmin | Dec 5, 2022 | Health Tips
Reviewed By: Evan Peterson PT, DPT
Ankle sprains are one of the most common injuries and occur in a variety of different settings. Whether it is a young athlete or an individual who rolls their ankle by missing a step, many will experience and ankle sprain at least once in their lifetimes. Chronic Ankle Instability or CAI is typically caused by repetitive lateral ankle sprains and can result in articular changes or degenerative osteoarthritis in the ankle. The ankle is an important joint for walking and balance and in order to perform both tasks well, a person must be able to utilize various neuromuscular strategies which include both feedback and feedforward control. In its simplest terms, feedback control is reactive whereas, feedforward control is proactive. Feedback control is our body’s ability to respond to a changing environment and feedforward control is our body’s ability to prepare for an environment we expect. It is proposed that those with CAI have deficits in both feedback and feedforward neuromuscular control. What this means for preventing reoccurring ankle injury is that a person with CAI may have difficulty adjusting their foot and ankle posture to create stability while attempting functional or recreational activities.
Yen et al. 2016 wanted to confirm their belief that people with CAI have impairments in their feedforward and feedback control during walking. Previously, they conducted a similar study testing feedback control of healthy subjects while walking. They found significant increase in ankle positioning (less inversion) while walking due to external loads.
Methods
The authors selected 12 students from Northeastern University who had no significant differences. The subjects filled out a Cumberland Ankle Instability Tool (CAIT) to determine the severity of their recurring ankle sprain. In this study, recurring ankle sprain was defined as at least 2 ankle sprains in the past 6 months. Control subjects scored highly on the CAIT and did not report ankle sprain in the past year. Ankle movement was captured via a motion capture system comprising of 6 cameras. Patients were asked to walk on a treadmill at a self-selected comfortable pace for 3 separate conditions. The first condition acted as a baseline, the second was the intervention phase in which sandbags were placed on the subject’s lateral metatarsal bones, forcing inversion, and the third condition had the bags removed.
Results
The baseline condition showed no significant difference between amount of inversion; however, the CAI group had a trend toward more inversion. During the intervention phase of the trial, both groups showed a change in the amount of eversion over a period of time. The group without CAI had increased eversion throughout the trial whereas the CAI group originally corrected to a more everted position but soon returned to baseline measures. After the weights were removed in the third condition, the increase in ankle eversion carried over in the control group. The CAI group showed a return to baseline suggesting no after effect from the external load.
Discussion
The results show that with external load both the control group and the group with CAI are able to respond to changes in their environment but the CAI group has difficulty doing so for a prolonged amount of time. The authors of this article were unable to identify a specific reason for this occurrence, but were able to formulate a few hypotheses. First is that the individuals were able to detect changes in the environment, but overtime became less sensitive to these changes. A less likely explanation is that the individuals with CAI have decreased everter muscle strength and endurance. These results suggest feedback control is somewhat diminished in those with CAI. The period in which the sandbags were removed was utilizing to assess a person’s ability to rely on feedforward control. The authors believe due to small changes in the after effect further studies should be conducted to determine the quality of feedforward control in those with CAI.
Physical Therapy First
At Physical Therapy First, our therapists are trained to develop exercises and assess a patient’s strategies when balancing or walking. Following ankle sprain or recurring ankle sprains it can be important to practice utilizing your feedback and feedforward controls in order to retrain your ankle and foot musculature for prevention of future ankle sprain. If you are struggling with an ankle that continues to roll with sports or with household tasks, please contact us and we will be happy to assist you.
Reference:
Feedback and Feedforward Control During Walking in Individuals With Chronic Ankle Instability (jospt.org)
by ptfadmin | Nov 28, 2022 | Health Tips
by Tyler Tice, PT, DPT, MS, ATC
Introduction:
Over the last few decades, the treatment options for Parkinson’s disease (PD) has significantly improved, resulting in effectively prolonged period of time people with PD live with disability. Due to this, the role of effective physical therapy (PT) and rehabilitative management for people with PD has greatly increased. PD affects dopamine within the brain, resulting in the presence of motor symptoms such as tremors and bradykinesia (slow movement) and non-motor symptoms such as changes in mood and changes in sense of smell. Diagnosis of PD is usually made after the classical motor signs of bradykinesia, rigidity, tremor, and postural instability (balance issues) emerge. Currently, there is no neuroprotective treatment for PD available so medical treatment is focused on treating the symptoms. As PD is projected to continue affecting higher numbers of our population as well as younger individuals, there is a need for effective non-pharmacological treatment early in the course of the disease. This review investigates the effects of a variety of modes of exercise and PT in the treatment of PD.
Aerobic Training:
Moderate to high intensity aerobic training may be the most beneficial in managing motor symptoms, improving physical function, and reducing disability in persons with PD. Studies where treadmill training was completed demonstrated better results regarding improvements in walking, most likely due to the intensity in which it could be completed, however, cycling is a viable option for persons with PD where walking may not be a safe option when initially beginning aerobic exercise. Additional research needs to be completed regarding the effect of aerobic exercise on non-motor symptoms, however existing research is promising as one study showed an improvement in executive function (higher level thinking needed to plan and carry out tasks), attention, and memory after one month of treadmill training.
Resistance Training:
Moderate to high intensity resistance exercise focused on movement speed or muscle power production may be beneficial in reducing disease severity, improving physical function, and reducing disability. One study demonstrated an improvement in cognition in addition to strength and mobility after the 2-year course of the study, suggesting long-term motor and non-motor benefit of participating in resistance exercise. Multiple studies also demonstrated benefit of resistance exercise when specific functional limitations such as climbing stairs or standing from a chair were targeted. Additional research is still needed to investigate the benefit of resistance exercise, especially in relation to their effects on non-motor symptoms.
Balance Training:
For persons with mild to moderate PD, balance training has demonstrated a significant ability to reduce fall rates. Additionally, studies that were clinic-based rather than home-based provided a greater level of supervision and intensive training, resulting in greater reductions in fall rates. Balance training also improved non-motor symptoms such as reductions in pain, depression, and apathy. However, it is important to note that in patients with severe PD appeared to have an increase in falls rate following participation in balance training. What causes this increase is unknown but may be attributed to increased gait-related mobility without an improvement in postural control or increased exposure conditions that challenge the individual’s balance without having the skills to manage these challenges.
Gait Training:
Gait training is effective in improving various aspects of walking in persons with PD. Treadmill training and moderate intensity overground walking have been shown to improve gait speed, walking capacity, and step/stride length. This is important as gait is not primarily impacted by current pharmacological treatments for PD. Providing cueing while ambulating has also been shown to improve various aspects such as giving auditory cues for gait speed or auditory and visual cues for freezing of gait. Dual-tasking such as walking and talking or walking and carrying an object is an aspect of ambulation that can be difficult for persons with PD. Practicing dual-tasking in a safe and controlled environment is effective in improving walking under dual-tasking conditions.
Physical Therapy:
Despite the evidence that supports early and regular exercise intervention in persons with PD, the utilization of PT services in the US is remarkably low. There are many factors that may contribute to this such as insurance coverage and other medical provider knowledge on the benefit of exercise and PT in persons with PD. Typically, to justify the need for PT to insurance companies, the patients must demonstrate functional improvement in order to continue with PT, however, policy and guideline changes have been implemented to improve access to PT for persons with PD. By initiating PT earlier in the disease process, more preventative measures can be taken, which ultimately will positively impact the quality of life of the individual.
Secondary Prevention Model:
Once initially diagnosed with PD, patients consult with a PT with expertise in PD. The PT performs what is referenced as a clinical battery of tests to establish a baseline level of function that can be tracked throughout the disease course. In the first few visits, the PT will prescribe an exercise program that is tailored to the individual and give them the tools to be success in consistently completing the program. A critical element of this approach is regular follow-up visits. Just as regular visits to the neurologist are necessary for reassessment of PD symptoms so appropriate adjustments to medication can be made, regular follow-up visits to a PT allow for reassessment of functional status and necessary adjustments to their exercise program to address changes in symptom presentation. There has also been an increase in community-based exercise programs, which further expands access to physical activity. These exercise programs can vary in intensity, however regular follow-up visits to PT can allow PTs to assist in finding programs that appropriately challenge their patient.
Take Home Message:
Regular exercise is highly beneficial for persons with PD. The advantage of beginning PT early in disease progression is that it can help mitigate the extent to which the motor and non-motor symptoms impact daily life. Additionally, if there were to be a change in function, receiving PT treatment can directly help with being able to successfully complete functional tasks such as climbing stairs to promote safe independence of persons with PD.
Article Reference:
Ellis, T. D., Colón-Semenza, C., DeAngelis, T. R., Thomas, C. A., Hilaire, M. S., Earhart, G. M., & Dibble, L. E. (2021). Evidence for Early and Regular Physical Therapy and Exercise in Parkinson’s Disease. Seminars in neurology, 41(2), 189–205. https://doi.org/10.1055/s-0041-1725133
by ptfadmin | Nov 21, 2022 | Health Tips
by Tyler Tice, PT, DPT, MS, ATC
Introduction:
Over 700,000 total knee arthroplasty (TKA) surgeries are performed each year in the US with this number expected to increase to over 3 million by 2030. A TKA is typically performed to reduce knee pain as well as self-reported physical function ability. However, even when considered full recovered 12 months after surgery, patients’ physical function when formally measured by performance-based measures and quadriceps strength are rarely improved compared to pre-surgery function. As shown in previous research, post-op protocols that include strengthening and functional exercises that are progressed based on clinical milestones promotes better outcomes compared to protocols that lack these interventions. However, there is no current research that compares patients who completed a progressive strengthening post-op protocol to healthy age-matched peers, which makes it difficult to determine whether these protocols are effective in fully restoring physical function. As younger, more active populations begin to undergo TKA surgeries, it’ll be imperative to know whether these progressive strengthening interventions are effective in restoring the level of physical function required to return to physically demanding occupations and recreational activities.
Methods:
This study investigated at 205 participants who underwent a unilateral primary TKA for knee osteoarthritis (OA). Additionally, 88 participants were recruited to serve as the healthy age-matched control group. Exclusion criteria for both groups can be found in the original article. Participants who underwent a TKA were randomized into one of three groups: progressive strengthening rehabilitation, progressive strengthening rehabilitation plus neuromuscular electrical stimulation for the quadriceps, or standard of care. All participants received inpatient rehabilitation in the hospital, followed by home and outpatient PT. Participants in the progressive strengthening rehabilitation groups completed at least 12 outpatient PT visits at the University of Delaware Physical Therapy clinic. Treatment focused on addressing the physical impairments after TKA as well as progressive strengthening exercises that targeted muscle groups in the lower extremity. Participants in the standard of care group attended other physical therapy clinics in the community and completed an average of 23 outpatient PT sessions with no set guidelines for clinicians to follow. Treatment primarily consisted of range of motion (ROM) exercises, stationary cycling, and various straight-leg exercises.
Outcome measures:
The Knee Outcome Survey – Activity of Daily Living (KOS-ADL), active knee ROM, maximal voluntary isometric contraction (MVIC) of the quadriceps, the Timed Up and Go (TUG), stair climbing time (SCT), and 6-minute walk (6MW) test were measured 12 months following surgery as well as in the control group to compare between groups.
Results:
There was a significant between-group effect for all clinical variables.
A higher proportion of participants in the progressive strengthening group achieved the lower bound cut-off for knee extension ROM, quadriceps strength, and SCT compared to the standard of care group.
Participants in the progressive strengthening group were 2-4 times more likely to achieve performance above the lower bound of the of the confidence interval of the control group for knee extension angle, performance on SCT, and quadriceps strength.
The percentage of participants in the progressive strengthening group that achieved the lower bound cutoff in at least one of the seven variables analyzed was greater compared to the standard of care group (67% vs. 47.5%).
Discussion:
Similar to previous research, participants who underwent a TKA demonstrated worse self-reported scores, greater physical impairments, and lower performance-based outcomes compared to the control group. However, a greater proportion of patients in the progressive strengthening protocol achieved what could be considered normal clinical and functional scores when evaluating the outcomes individually. This suggests that patients who follow a progressive strengthening protocol post-TKA may improve their likelihood of achieving normal age-matched outcomes. Also, a greater proportion of participants in the progressive strengthening group achieved the lower bound cut-off for quadriceps strength, knee extension angle, and SCT, suggesting progressive exercises may be more effective in optimizing outcomes after TKA.
It’s important to note that all participants still had substantial impairments 12 months after surgery compared to the control group. Failing to restore function by 12 months after surgery may overall impact the patient’s ability to achieve normal function as progress measured by outcome measures typically plateaus around 12 months post-surgery. There are many factors that may contribute to this such as pre-operative function, lack of consensus between providers regarding rehabilitation protocol and surgical procedure. Regardless, this highlights the importance of including the inherent limitations of the surgical procedure and post-op rehabilitation at restoring normal function for patients with end-stage OA when educating patients.
Take Home Messages:
TKA is a surgery that is becoming increasingly more common as time goes on and research has consistently showed that after surgery, it is difficult for patients to achieve pre-surgery function that can be comparable to age-matched peers without knee pathology. As more active patients begin to undergo this surgery, it’ll be important that they are able to achieve pre-surgery function to enable them to participate in recreational activity or more physically demanding occupations. While this study showed that overall, all participants demonstrated worse functional outcomes compared to the control group, participants in the progressive strengthening group demonstrated better functional outcomes compared to the standard of care group. This suggests that the inclusion of these exercises may be beneficial to the functional recovery of TKA patients. There are still many other factors that may be contributing to why TKA patients have difficulty recovering to their pre-surgery function, which emphasizes the role of patient education in the recovery process to set realistic expectations for these patients while also enabling them to recover to their greatest ability.
Article Reference:
Pozzi, F., White, D. K., Snyder-Mackler, L., & Zeni, J. A. (2020). Restoring physical function after knee replacement: a cross sectional comparison of progressive strengthening vs standard physical therapy. Physiotherapy theory and practice, 36(1), 122–133. https://doi.org/10.1080/09593985.2018.1479475
by ptfadmin | Nov 14, 2022 | Health Tips
Reviewed by Mark Boyland PT, DPT, CSCS
This study sought to explore the effect times of manual therapy alone vs therapeutic exercise alone as well as to break down and compare the effects of these two interventions in the short and mid term.
The authors compared visual analog scale, pressure pain threshold, cervical disability through the Neck Disability Index Outcomes. These values were assessed at evaluation, week 1, week 4, and week 12.
The participants were split into 1 of 3 intervention groups; Manual Therapy, Therapeutic Exercise, or Sham. At the end of the trial the study was able to analyze date across 67 participants, 22 in the Manual Therapy Group, 23 in the Therapeutic Exercise Group, and 20 in the Sham treatment group. Demographic date was relatively similar between groups, however there were more female participants than males.
The interventions were listed for each group. The manual therapy group included frequency of interventions, grading of mobilizations/manipulations, speed of mobilization, duration of mobilization, and sets of mobilizations. The therapeutic exercise group include progressions of exercises from week 1 and 2 and the exercises after week 2. Exercise descriptions included patient position with equipment required, and duration/frequency of exercises. The authors also provided a description for how the sham treatment was provided. It is noted that the sham treatment group did receive either manual therapy or therapeutic exercise interventions only after completion of the study. The study was conducted by researchers from the University of Seville, Seville, Spain and potential mistranslations may be present when reviewing the applied interventions.
The intervention groups had significant improvements in VAS at weeks 1,4, and 12. Both intervention groups had significant changes for the NDI at weeks 1 and 4. However, the manual therapy group was able to maintain these improvements into week 12 with no statistical difference and the therapeutic exercise group had a poorer score relative to the 4 week evaluation however the 12 week score was still lower than the patient’s initial score. The pain pressure threshold was only reduced in the manual therapy group at 4 weeks, however at 12 weeks both intervention groups showed improvements. The control group demonstrated no significant changes throughout the study.
In regards to selection of these interventions as stand alone treatments, therapeutic exercise may improve function more quickly whereas manual therapy may improve pain more quickly, both interventions can have similar results in the mid term. The authors note that a larger sample size may refute their findings and that treatment of chronic non specific neck pain should include multiple interventions not limited to only manual therapy and therapeutic exercise but could also include patient education and pain science education. The authors also note that there is no method that guarantees patients complete their home exercises.
For patients: Physical therapy for non specific chronic neck pain can be treated with hands on and an exercise approach and there can be significant changes made within just 4 weeks that can last up to twelve weeks but there is some work on your part that has to be done as well in the short, mid, and long-term
by ptfadmin | Nov 7, 2022 | Health Tips
Article Review: by Kira Zarzuela, SPT, Tyler Tice, PT, DPT, OCS
Background:
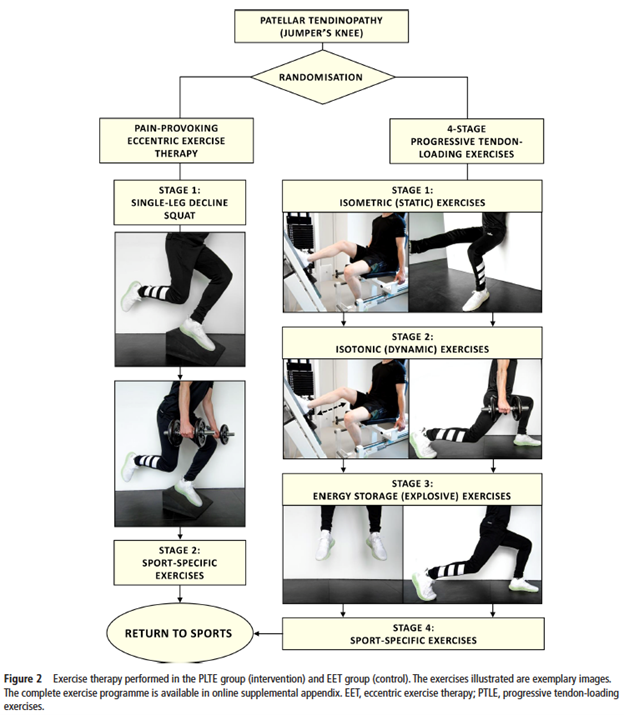
Patellar tendinopathy (PT) is a common chronic tendon injury that not only effects a high percentage of the athletic population, but also a number of people that participate in physically demanding work. Currently, there is no known direct cause of PT, making it difficult to determine first-line treatment as not all people respond the same way to the same treatments. Eccentric exercise therapy (EET) is one line of treatment that has strong evidence supporting its effectiveness for PT, however, EET can be pain-provoking. Additionally, the onset of pain with this mode of treatment makes its use debatable during the competitive season for athletes as they are less likely to adhere to treatment. Recent research proposes the utilization of progressive tendon-loading exercises (PTLE) within the limits of “acceptable” pain, however, there is no current comparison between EET and PTLE. This study compares the effectiveness of PTLE with EET in patients with PT.
Methods:
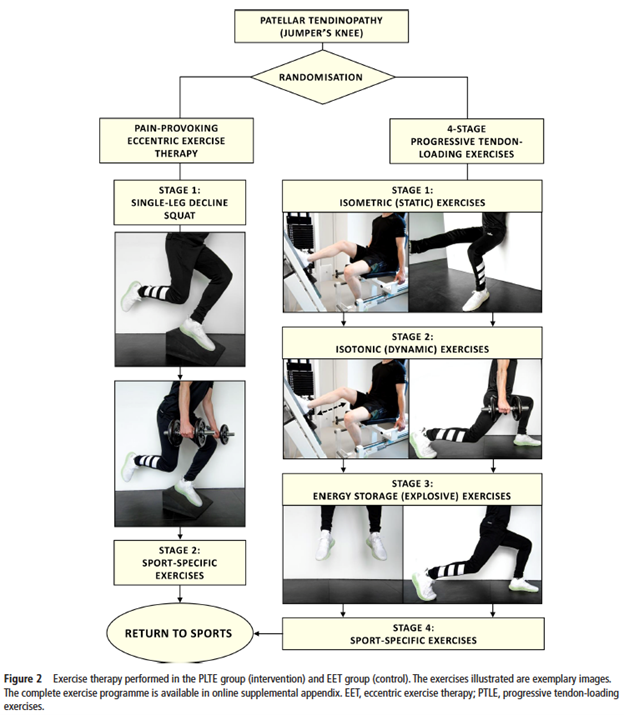
This study looked at 76 recreational, competitive, and professional athletes with clinically diagnoses and ultrasound-confirmed PT that were randomly assigned to receive either EET (control group) or PTLE (intervention group) for 24 weeks. Most participants (82%) had previously underwent treatment for PT but failed to recover fully. PTLE consisted of 4 stages: 1. daily isometric exercises, 2. isometric and isotonic exercises, 3. plyometric loading and running exercises, and 4. sport-specific exercises. Progression through these stages was determined by individual progression criteria based on pain provocation during a single-leg squat. EET consisted of 2 stages: eccentric exercises performed 2x/day for 12 weeks followed by sport-specific exercises for 12 weeks if the participant was compliant to stage 1. Both groups received exercises targeting risk factors for PT such as flexibility exercises and hip strengthening exercises.
Outcome measures:
The primary outcome was the VISA-P questionnaire. Secondary outcomes were return to sport rate, subjective patient satisfaction, and exercise adherence.
Results:
The improvement in VISA-P score was significantly better for PTLE than for EET after 24 weeks (28 points vs. 18 points).
There was a trend towards a higher return to sports rate in the PTLE group (43% vs. 27%).
The percentage of patients with an excellent satisfaction was significantly higher in the PTLE group (38%) than in the EET group (10%).
There was no significant difference between subjective patient satisfaction and exercise adherence between the PTLE and EET groups after 24 weeks.
Discussion:
This study demonstrated improved performance in the PTLE group compared to the EET group that was both important and clinically relevant. Additionally, as this study included participants who had received prior treatment for PT but did not improve, the findings of this study also indicate that PTLE is still beneficial to this population. Other findings from the PTLE group are that there was a higher return to sports rate compared to the EET group and participants in the PTLE group reported that the exercises were significantly less painful to perform. However, it should be noted that in the PTLE group, less than half of the patients returned to sports at a preinjury level after performing PTLE for 24 weeks. This indicates the need for further improvements on the PTLE program. Both groups demonstrated improvements in pain, function, and ability to play sports, suggesting the importance of exercise therapy in general as a form of conservative management for patients with PT.
Take Home Messages:
Patellar tendinopathy is a chronic condition that affects a large number of people, however there is constant research being conducted to investigate what forms of conservative treatment are the best to trial prior to more invasive procedures. At the time this study was conducted, eccentric exercise training, or training done where the muscle is loaded during the phase where its length is increasing, had strong evidence supporting the effectiveness in PT. The difficult part regarding EET is that it is pain-provoking and its beneficial use during a competitive season for an athlete was uncertain. Another challenge of PT is that one treatment doesn’t work for all patients diagnosed with PT, resulting in several patients having gone through an unsuccessful bout of physical therapy, which only adds to the frustration surrounding the rehabilitation process. This study demonstrated that progressive tendon loading not only worked the same, if not better, than EET and was less pain-provoking, but also was successful in participants who had gone through unsuccessful bouts of treatment for their PT. For clinicians, this means that utilization of progressive tendon loading should be trialed in patients with longer-standing PT or previously failed bouts of treatment. For patients, this means progressive tendon loading is worth trialing, regardless of chronicity or history of treatment, as a form of treatment for PT.
Article Reference:
Breda, S. J., Oei, E., Zwerver, J., Visser, E., Waarsing, E., Krestin, G. P., & de Vos, R. J. (2021). Effectiveness of progressive tendon-loading exercise therapy in patients with patellar tendinopathy: a randomised clinical trial. British journal of sports medicine, 55(9), 501–509. https://doi.org/10.1136/bjsports-2020-103403