by ptfadmin | Nov 7, 2023 | Health Tips
Reviewed by Jerome Thomas, SPT, Tyler Tice, PT, DPT, OCS, ATC
Manual therapy is one of the most common interventions utilized by physical therapists and generally refers to passively applying mechanical forces to the superficial body in order to receive a therapeutic effect. Manual therapy is often implemented in combination with other modalities and interventions to provide a comprehensive, multi-modal approach to musculoskeletal management. Additionally, manual therapy has shown superior clinical outcomes for numerous musculoskeletal disorders in the research that has been conducted on this intervention. However, new evidence in the field of physical therapy has led to a paradigm shift in the way that manual therapy can be utilized. Researchers in physical therapy are asking this pivotal question: Do some specific groups of individuals receive greater therapeutic benefits from manual therapy compared to others?
The International Association for the Study of Pain (IASP) outlines three major pain classifications: nociceptive, nociplastic, and neuropathic. Nociceptive pain is a protective mechanism, caused by physiological activation of pain receptors and is usually attributed to actual tissue damage such as stubbing your toe. Nociplastic pain is often described as increased sensitivity to pain due to the impaired functioning of the pain-processing systems in the central nervous system. This type of pain presentation is commonly seen in chronic conditions such as fibromyalgia. Lastly, neuropathic pain arises from nerve damage or irritation and can often be characterized as shooting, burning, or stabbing pain. There is a prevalent hypothesis that categorizing patients based on these three major pain presentations will allow physical therapists to better tailor their manual therapy techniques for improved patient outcomes.
This detailed study was a consensus-based survey design between the expert clinicians on manual therapy, with group members evaluating one of the three major pain presentations. These group members were tasked with developing an optimal manual therapy treatment framework for each specific pain presentation. These expert clinicians or stakeholders in this study all exhibited high levels of training and experience using manual therapy interventions in clinical practice. Each specific manual therapy framework would outline specific treatment protocols that could be modified based on the patient’s signs and symptoms. As expected, there are both differences and similarities between the theoretical frameworks of the three IASP mechanism-based pain classifications.
The experts came away with several conclusions concerning each specified theoretical framework. The neuropathic and nociplastic frameworks recommended a graded application scheme, with less aggressive techniques early in treatment to monitor patient response; the nociceptive framework recommended approaches that are more aggressive once the patient’s symptoms are improved. For the neuropathic and nociplastic frameworks, it was recommended that you attempt to reconceptualize the pain experience for these patients and create an environment that limits fear and catastrophizing. Additionally, there was an emphasis on “increasing space” for the neuropathic framework as nerve movement increases blood flow in nerve-related conditions.
Clinical Application:
All three frameworks recommended selecting a therapeutic manual therapy approach based on the patient’s unique pain presentation. Patients with neuropathic pain will benefit from graded application of manual therapy and techniques that aim to increase nerve movement for improved blood flow. Patients with nociplastic pain will generally benefit from a reconceptualized view of their pain experience along with less aggressive techniques early on in their treatment plan. Patients with nociceptive pain can be introduced to more aggressive techniques as their symptoms improve; techniques should be selected with the goal of increasing pain-free active range of motion.
Reference:
Cook, C. E., Rhon, D. I., Bialosky, J., Donaldson, M., George, S. Z., Hall, T., … & Puentedura, E. J. (2023). Developing Manual Therapy Frameworks for Dedicated Pain Mechanisms. JOSPT Open, 1(1), 1-15.
by ptfadmin | Oct 30, 2023 | Health Tips
Reviewed by Jerome Thomas, SPT, Tyler Tice, PT, DPT, OCS, ATC
Achilles tendinopathy is a very common, overuse injury of the lower extremity that often affects athletes and highly-active individuals that engage in activities such as running, jumping, and other recreational-related tasks. Achilles tendinopathy can consequently become detrimental to a patient’s activity levels and overall functional capacity as many patients may begin to decrease their activity in response to pain or decline in function. There are a very limited number of randomized controlled trials and established treatment protocols for Achilles tendinopathy, despite various forms of modalities and exercise utilized for this patient population. This prospective, randomized controlled trial attempted to evaluate the efficacy of utilizing the Pain-Monitoring Model in combination with a continued, tendon-loading training regimen for patients with Achilles tendinopathy.
In this study, 38 patients with Achilles Tendinopathy were divided into two separate treatment groups: an exercise training group (n=19) and an active rest group (n=19) that was not allowed to perform any physical activity for the first 6 weeks of rehabilitation. However, both treatment groups were rehabilitated with an identical, progressive Achilles tendon-loading program for 12 weeks to 6 months. As previously mentioned, the exercise training group was allowed to continue loading activities for the Achilles tendon in accordance with the Pain-Monitoring Model in the same timeframe that the active rest group was restricted .
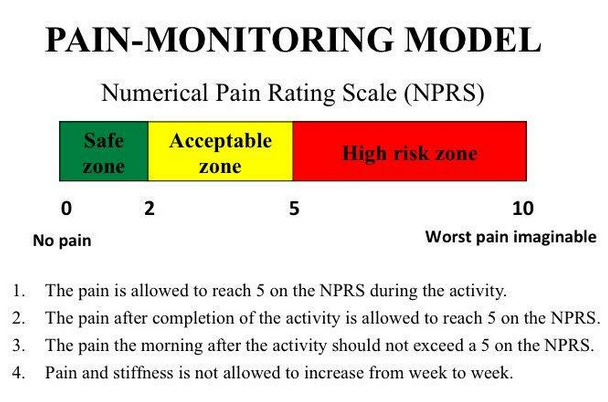
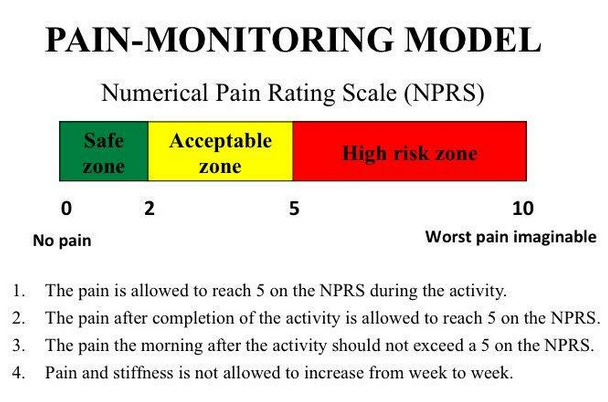
Guidelines for the Pain-Monitoring Model were modified by Silberngael et al. in their 2001 study. According to their guidelines for the pain-monitoring model, pain was not allowed to reach level 5 on the VAS where a 0 indicated no pain and a 10 indicated the worst pain imaginable. Pain after the exercises were allowed to reach a 5 on the VAS but should have subsided by the following morning. Additionally, pain and stiffness in the Achilles tendon were not allowed to increase from week to week. Treatment protocol consisted of a progressive, four-phase program that incorporated the following exercises: 2-legged, 1-legged, eccentric, and fast-rebounding toe raises. Phase 3 allowed the patients to transition to more plyometric-style movements if the subsequent phases were handled with no pain in the tendon insertion or increased morning stiffness. The primary outcomes utilized for the conclusion of this randomized controlled trial were the VISA-A-S score, which was a specialized Achilles assessment questionnaire, as well as pain with hopping measured with the VAS scale.
The results of the trial showed that both treatment groups showed significant improvements in VISA-A-S score and hopping pain in comparison to baseline measurements at 6 weeks, 3 month, 6 month, and 12 month evaluations. More importantly, this study could not demonstrate any negative findings or implications for allowing the patients in the exercise training group to continue Achilles tendon-loading activities in accordance with the Pain-Monitoring Model. Therefore, early implementation of strengthening exercises for the Achilles tendon and plantar flexor complex, as well as moderated activities such as running and jumping, can be utilized to reduce symptoms and improve functional capacity in patients with Achilles tendinopathy. In previous literature, it had been recommended that patients with Achilles tendinopathy take a rest period from the activities that were pain-provoking. However, this study demonstrates that those same activities can be continued as long as the patient with Achilles tendinopathy is following the protocols set by the Pain-Monitoring Model.
Clinical Application:
Based on this study, we can use the Pain Monitoring Model as a guide to help determine the appropriate amount of activity and exercise for the proper amount of loading to the Achilles tendon with Achilles tendinopathy without “overdoing it”. Below is a graphic that simplifies the explanation of this model:
Reference:
Silbernagel KG, Thomeé R, Eriksson BI, Karlsson J. Continued sports activity, using a pain-monitoring model, during rehabilitation in patients with Achilles tendinopathy: a randomized controlled study. Am J Sports Med. 2007 Jun;35(6):897-906. doi: 10.1177/0363546506298279. Epub 2007 Feb 16. PMID: 17307888.
by ptfadmin | Jun 27, 2023 | Health Tips
by John Baur, PT, OCS, FAAOMPT
Acetaminophen (APAP) is a commonly used over-the-counter pain reliever that can cause liver damage when taken in high doses. The common brand name for acetaminophen (APAP) is Tylenol and acute liver injury caused by APAP overdose is a serious medical condition that can lead to liver failure and death. Probiotics are live microorganisms that can provide health benefits when consumed in adequate amounts. Bacillus spp. spores are a type of probiotic that have been shown to modulate the gut microbiota and improve overall health. In this report, we will discuss a study that investigated the effects of a probiotic containing Bacillus spp. spores on a rat model of APAP-induced acute liver injury.
Methods
The study used a rat model of APAP-induced acute liver injury. The rats were divided into four groups: a control group, an APAP group, an APAP group treated with the probiotic, and an APAP group treated with N-acetylcysteine (NAC), a standard treatment for APAP-induced liver injury. The probiotic contained Bacillus spp. spores.
The rats were treated with the probiotic or NAC for a period of 3 days. The severity of liver injury was assessed by measuring levels of liver enzymes in the blood and examining liver tissue for signs of damage.
Results
The study found that treatment with the probiotic containing Bacillus spp. spores protected against APAP-induced acute liver injury in rats. The probiotic significantly reduced levels of liver enzymes in the blood and reduced signs of liver damage in the liver tissue. The protective effects of the probiotic were comparable to those of NAC, the standard treatment for APAP-induced liver injury.
The study also found that the probiotic increased the abundance of beneficial bacteria in the gut microbiota, which may have contributed to its protective effects on the liver.
Conclusion
The study suggests that treatment with a probiotic containing Bacillus spp. spores can protect against APAP-induced acute liver injury in rats. The probiotic reduced levels of liver enzymes in the blood and reduced signs of liver damage in the liver tissue. These findings suggest that Bacillus spp. spores could be a promising treatment option for APAP-induced liver injury in humans. Further research is needed to confirm these findings in human clinical trials, but the study provides a promising avenue for future research in the field of probiotics and liver health.
Physical Therapy First recognizes the importance staying well-informed with the latest health and wellness topics that affect our patients. Megasporebiotic made by Microbiome Labs (microbiomelabs.com) is the first spore-base probiotic with research which supports it use for Acetaminophen (APAP)-induced acute liver injury and many other health conditions.
Reference
Probiotic Bacillus Spores Protect Against Acetaminophen Induced Acute Liver Injury in Rats.Neag MA, Catinean A, Muntean DM, Pop MR, Bocsan CI, Botan EC, Buzoianu AD.Nutrients. 2020 Feb 27;12(3):632. doi: 10.3390/nu12030632.
by ptfadmin | Jun 12, 2023 | Health Tips
by John Baur, PT, OCS, FAAOMPT
Ulcerative colitis (UC) is a chronic inflammatory bowel disease that affects the colon and rectum. It is characterized by symptoms such as abdominal pain, diarrhea, and rectal bleeding. While the exact cause of UC is unknown, it is believed to be related to an imbalance in the gut microbiota and inflammation. Probiotics are live microorganisms that can provide health benefits when consumed in adequate amounts. Bacillus spp. spores are a type of probiotic that have been shown to modulate the gut microbiota and improve overall health. In this report, we will discuss a study that investigated the effects of a probiotic containing Bacillus spp. spores, amino acids, and immunoglobulins on a rat model of UC.
Methods
The study used a rat model of UC induced by dextran sulfate sodium (DSS). The rats were divided into four groups: a control group, a DSS group, a DSS group treated with the probiotic, and a DSS group treated with mesalazine, a standard treatment for UC. The probiotic contained Bacillus spp. spores, amino acids, and immunoglobulins.
The rats were treated with the probiotic or mesalazine for a period of 14 days. The severity of UC was assessed by measuring body weight, stool consistency, and rectal bleeding. The inflammatory response was assessed by measuring levels of inflammatory cytokines in the colon tissue.
Results
The study found that treatment with the probiotic containing Bacillus spp. spores, amino acids, and immunoglobulins exerted protective effects on the rat model of UC. The probiotic significantly reduced the severity of UC, as evidenced by improvements in body weight, stool consistency, and rectal bleeding. The probiotic also reduced the inflammatory response, as evidenced by reductions in levels of inflammatory cytokines in the colon tissue.
Conclusion
The study suggests that treatment with a probiotic containing Bacillus spp. spores, amino acids, and immunoglobulins can exert protective effects on a rat model of UC. The probiotic reduced the severity of UC and the inflammatory response, suggesting that it could be a promising treatment option for UC. Further research is needed to confirm these findings in human clinical trials, but the study provides a promising avenue for future research in the field of probiotics and UC treatment.
Physical Therapy First recognizes the importance staying well-informed with the latest health and wellness topics that affect our patients. Megasporebiotic made by Microbiome Labs (microbiomelabs.com) is the first spore-base probiotic with research which supports it use for Ulcerative colitis (UC) and many other health conditions.
Reference
Probiotic Bacillus Spores Together with Amino Acids and Immunoglobulins Exert Protective Effects on a Rat Model of Ulcerative Colitis. Catinean A, Neag MA, Krishnan K, Muntean DM, Bocsan CI, Pop RM, Mitre AO, Melincovici CS, Buzoianu AD. Nutrients. 2020 Nov 24;12(12):3607. doi: 10.3390/nu12123607.
by ptfadmin | Jun 5, 2023 | Health Tips
By John Baur, PT, DPT, OCS, FAAOMPT
The gut microbiota plays a crucial role in maintaining overall health and well-being. An imbalance in the gut microbiota has been linked to a variety of health problems, including gastrointestinal disorders, metabolic disorders, and immune dysfunction. Probiotics are live microorganisms that can provide health benefits when consumed in adequate amounts. Bacillus spp. spores are a type of probiotic that have been shown to modulate the gut microbiota and improve overall health. In this report, we will discuss a study that investigated the effects of a spore-based probiotic containing five strains of Bacillus on the gut microbiota in a SHIME® model of the human gastrointestinal system.
The study used a SHIME® (Simulator of the Human Intestinal Microbial Ecosystem) model to simulate the human gastrointestinal system. The SHIME® model consists of five compartments that simulate different parts of the gastrointestinal tract, including the stomach, small intestine, and colon. The model was inoculated with fecal samples from healthy human donors to establish a complex and diverse gut microbiota.
The spore-based probiotic containing five strains of Bacillus (Bacillus subtilis, Bacillus clausii, Bacillus coagulans, Bacillus licheniformis, and Bacillus pumilus) was added to the SHIME® model for a period of 21 days. The metabolic activity and community composition of the gut microbiota were analyzed before and after treatment with the probiotic.
The study found that treatment with the spore-based probiotic containing five strains of Bacillus induced changes in the metabolic activity and community composition of the gut microbiota in the SHIME® model. Specifically, the probiotic increased the production of short-chain fatty acids (SCFAs), which are important for maintaining gut health and reducing inflammation. The probiotic also increased the abundance of beneficial bacteria such as Bifidobacterium and Lactobacillus, while reducing the abundance of harmful bacteria such as Clostridium difficile.
In conclusion, the study provides evidence that treatment with a spore-based probiotic containing five strains of Bacillus can induce changes in the metabolic activity and community composition of the gut microbiota in a SHIME® model of the human gastrointestinal system. The probiotic increased the production of short-chain fatty acids and the abundance of beneficial bacteria, while reducing the abundance of harmful bacteria. These findings suggest that Bacillus spp. spores could be a promising treatment option for a variety of health problems related to gut microbiota imbalance, including gastrointestinal disorders, metabolic disorders, and immune dysfunction. Further research is needed to confirm these findings in human clinical trials, but the study provides a promising avenue for future research in the field of probiotics and gut health.
Physical Therapy First recognizes the importance staying well-informed with the latest health and wellness topics that affect our patients. Megasporebiotic made by Microbiome Labs (microbiomelabs.com) is the first spore-base probiotic with research which supports it use for maintaining gut health and reducing systemic inflammation.
Reference
Food Res Int. 2021 Nov; 149:110676. doi: 10.1016/j.foodres.2021.110676. Epub 2021 Aug 30.
Treatment with a spore-based probiotic containing five strains of Bacillus induced changes in the metabolic activity and community composition of the gut microbiota in a SHIME® model of the human gastrointestinal system. Massimo Marzorati, Pieter Van den Abbeele, Sarah Bubeck, Thomas Bayne, Kiran Krishnan, Aicacia Young
by ptfadmin | May 30, 2023 | Health Tips
By John Baur, PT, DPT, OCS, FAAOMPT
Irritable bowel syndrome (IBS) is a common gastrointestinal disorder that affects millions of people worldwide. It is characterized by symptoms such as abdominal pain, bloating, and changes in bowel habits. While the exact cause of IBS is unknown, it is believed to be related to an imbalance in the gut microbiota and inflammation. In recent years, there has been growing interest in the use of probiotics and other microbiota-targeted therapies for the treatment of IBS. In this report, we will discuss the potential of Bacillus spp. spores as a promising treatment option for patients with IBS.
Bacillus spp. Spores and Gut Microbiota
Bacillus spp. are a group of spore-forming bacteria that are commonly found in soil and water. They are known for their ability to survive in harsh environments and have been used for centuries in traditional medicine for the treatment of various ailments. In recent years, there has been growing interest in the use of Bacillus spp. spores as a probiotic for the treatment of gastrointestinal disorders.
Studies have shown that Bacillus spp. spores have the ability to modulate the gut microbiota and reduce inflammation. They have been shown to increase the abundance of beneficial bacteria such as Bifidobacterium and Lactobacillus, while reducing the abundance of harmful bacteria such as Clostridium difficile. Bacillus spp. spores also produce short-chain fatty acids (SCFAs), which are important for maintaining gut health and reducing inflammation.
Bacillus spp. Spores and Irritable Bowel Syndrome
Several studies have investigated the potential of Bacillus spp. spores as a treatment option for patients with IBS. A randomized, double-blind, placebo-controlled trial found that a combination of Bacillus coagulans and fructooligosaccharides (FOS) significantly improved symptoms of IBS, including abdominal pain, bloating, and stool consistency. Another study found that Bacillus clausii spores significantly reduced symptoms of IBS, including abdominal pain and bloating.
The mechanism by which Bacillus spp. spores improve symptoms of IBS is not fully understood. However, it is believed that their ability to modulate the gut microbiota and reduce inflammation plays a key role. Bacillus spp. spores may also improve gut barrier function, which is important for preventing the entry of harmful bacteria and toxins into the bloodstream.
In conclusion, Bacillus spp. spores have shown promising results as a treatment option for patients with irritable bowel syndrome (IBS). Studies have shown that Bacillus spp. spores have the ability to modulate the gut microbiota and reduce inflammation, which are key factors in the development of IBS. Bacillus spp. spores have been shown to improve symptoms of IBS, including abdominal pain, bloating, and stool consistency. While more research is needed to fully understand the mechanism by which Bacillus spp. spores improve symptoms of IBS, they offer a promising treatment option for patients who do not respond to traditional therapies. Bacillus spp. spores are generally safe and well-tolerated, making them a viable option for long-term use.
Physical Therapy First recognizes the importance staying well-informed with the latest health and wellness topics that affect our patients. Megasporebiotic made by Microbiome Labs (microbiomelabs.com) is the first spore-base probiotic with research which supports it use for IBS and many other health conditions.
Reference
Bacillus spp. Spores-A Promising Treatment Option for Patients with Irritable Bowel Syndrome.
Catinean A, Neag AM, Nita A, Buzea M, Buzoianu AD.Nutrients. 2019 Aug 21;11(9):1968. doi: 10.3390/nu11091968.