Glenohumeral Extension on the Dip: Considerations for the Strength and Conditioning Professional
by Nick Mattis, SPT
Introduction:
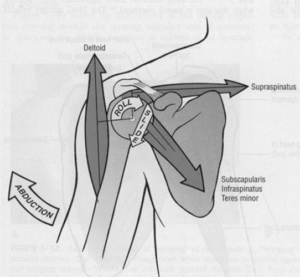
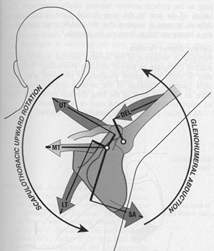
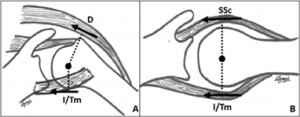
The glenohumeral joint (shoulder) has a high level of mobility which comes at a price of low stability. Due to the extensive range of motion of the shoulder, the shoulder is not as stable as several other joints in the body (i.e. elbow, knee). Passive stabilizers of the glenohumeral joint include which of the following? There are several passive stabilizers of the joint such as the glenoid labrum, the ligamentous structures, and the bony articulation of the joint (2). Active stabilizers of the glenohumeral joint include which of the following? Then there are active stabilizers of the joint such as rotator cuff muscles, deltoid, biceps brachii, and latissimus dorsi. These active stabilizers are able to contract to assist with keeping the humeral head in the glenoid fossa. Active and passive stabilizers can become strained/torn/ruptured when the humeral head enters abnormal positioning outside the center of the glenoid cavity. During the dip exercise the humerus often reaches the end range of extension and can place the humeral head in an abnormal position. Which of the following describes the movement of the humeral head at the end of a range of movement during a dip exercise? As the humerus rotates posteriorly as the arm goes back, the head of the humerus translates anteriorly. To keep the humerus from slipping out of the glenoid cavity, the active and passive stabilizers resist excessive anterior movement of the humeral head. The main active stabilizer preventing the excessive anterior translation in the dip is the clavicular head of the Pectoralis Major (PM). The passive stability to the anterior translation is produced by the Anterior Band of the Inferior Glenohumeral Ligament (AB-IGHL). During the dip exercise, which of the following tissues are of particular concern regarding injury and subsequent lack of joint stability? The PM and the anteroinferior joint capsule are the tissues of highest concern to be injured. The Pectoralis Major and the AB-IGHL receive the highest amount of stress on them in the bottom of the dip position. Damage to these structures can result in Anterior Instability of the glenohumeral joint.
Pectoralis Major:
Damage to the PM can result in a strain of the muscle. The clavicular head of the PM is assists in flexion of the GH joint. Which muscle is responsible for controlling the depth of the movement during the dip exercise? When performing a dip, this portion of the PM is actively elongating to eccentrically control the speed and depth at which the dip is performed. Glenohumeral movements that are at the highest risk of injury include which of the following three events? There have been three risk factors identified that can result in injury of the PM: 1) external rotation of the shoulder while in the end range of extension, 2) moderate to maximal loads placed on the PM, 3) eccentric contraction of the muscle (3).
Anterior Shoulder Instability:
Anterior Instability (AI) occurs when there is laxity either the active and/or passive stabilizers on the anterior surface of the GH joint. This can result in an anterior dislocation or subluxation of the joint. Repetitive loading of the passive AB-IGHL (performing dips frequently at high loads) can result in deformation of the ligament and lead to AI due to the excessive load at end ranges of extension combined with and externally rotated positioning. Similarly, injury to the active stabilizers can also result in AI. During exercise when the humeral head is pushed forward (anteriorly), which of the following rotator cuff muscles is responsible for actively contracting to resist this movement? The subscapularis and teres minor of the rotator cuff are recruited in end ranges of extension to reduce the amount of anterior translation of the humeral head.
The Dip:
Which of the following accurately describes the dip exercise? The dip is classified as a closed-kinetic-chain exercise that is performed at body weight, with the use of a band to reduce body weight, or the addition of a weight belt to add body weight. When considering the potential risk of injury during and prescription of the dip exercise, which of the following is recommended by the authors? Tips for the prescription of dips include limiting the depth of the dip to avoid the end range positon to reduce stress placed on the PM and AB-IGHL. The authors recommend within session programming variation for the purpose of? Repetitions, load, frequency, and rest time should all be managed and to reduce muscular fatigue. Reducing muscular fatigue will prolong the technique of the dip. Poor technique can often result in the 3 risk factors mention before that result in the highest risk of injury.
Physical Therapy First:
Here at Physical Therapy First, our team of skilled therapists are able to assist you in the recovery from shoulder instability. Through manual techniques and other interventions, we can restore your ROM, increase strength, and return you back to activity. Your therapist can help you properly decide whether exercises such as the dip are appropriate for you based on your individual functional needs. Call today to schedule an appointment.
References:
1) McKenzie, Alec K. BClinSci; Crowley-McHattan, Zachary J. PhD; Meir, Rudi PhD, CSCS; Whitting, John W. PhD; Volschenk, Wynand BA (HMS Hons) Sports Science, CSCS Glenohumeral Extension and the Dip: Considerations for the Strength and Conditioning Professional, Strength and Conditioning Journal: February 2021 – Volume 43 – Issue 1 – p 93-100 doi: 10.1519/SSC.0000000000000579
2) Terry GC, Hammon D, France P, Norwood LA. The stabilizing function of passive shoulder restraints. Am J Sports Med 19: 26–34, 1991.
3) Provencher CMT, Handfield K, Boniquit NT, et al. Injuries to the pectoralis major muscle: Diagnosis and management. Am J Sports Med 38: 1693–1705, 2010.