Physical Therapy Examination for the Diagnosis of Cervicogenic Headaches
What is a cervicogenic headache?
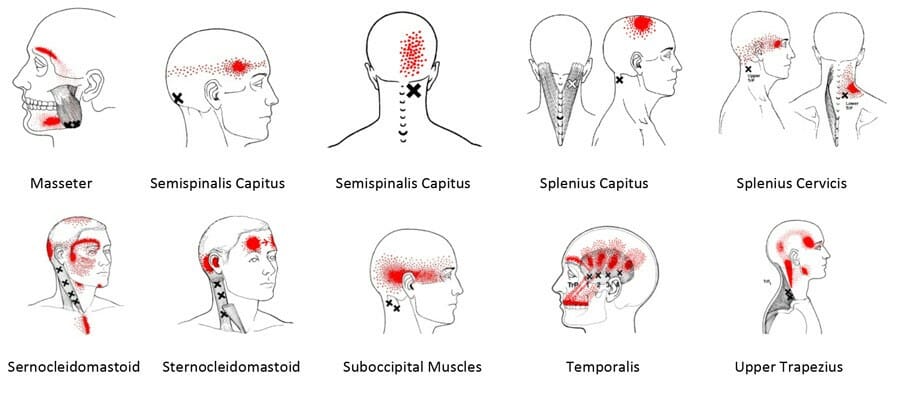
- At some point in their lives, ~96% of people will experience headaches. The cause of headaches may be unknown, due to another condition, or due to referred pain from an adjacent area of the body such as the ears, neck, or facial structures including the mouth and nose. A cervicogenic headache is a headache that results from a musculoskeletal impairment in the upper part of the neck, known as the upper cervical spine. Cervicogenic headaches stem from a dysfunction in the complex nervous system connections between the trigeminal nerve (a nerve the originates in the region between the spinal cord and the brain) and the nerves of the upper cervical spine. This dysfunction causes neck pain to refer to different areas of the head, resulting in a headache. People will often experience referred pain around one or both eyes as well.
How are cervicogenic headaches diagnosed?
- Cervicogenic headaches are typically diagnosed through a subjective examination, also known as a patient interview, and an objective examination during which a physical therapist examines the cervical spine and uses tests and measures to determine the cause of the patient’s headaches. According to a systematic review by Rubio-Ochoa et al., a physical examination of the cervical spine for a patient presenting with cervicogenic headaches should consist of sensitive tests such as accessory motion testing (PAIVMs) of the joints of the upper cervical spine as well as specific tests such as the cervical flexion-rotation test. During this test, the therapist will bend your head forward and rotate it side to side while monitoring any changes in your symptoms. The use of these tests assists the therapist in accurately diagnosing cervicogenic headaches and can guide treatment planning. Cervicogenic headaches have been shown to respond well to physical therapy intervention, so an accurate diagnosis is essential.
How can Physical Therapy First help with cervicogenic headaches?
- Here at Physical Therapy First, we will evaluate you to determine the cause of your headaches and the best approach to treating them. Your initial examination will begin with a subjective interview during which the physical therapist asks questions about your headaches, any neck pain, and other pertinent medical history. The physical therapist will then conduct a physical examination that includes evidence-based tests and measures such as the ones mentioned above. The physical therapist will then develop a comprehensive, individualized treatment plan consisting of exercises and manual therapy to help alleviate your cervicogenic headaches and other symptoms.
Reference
Rubio-Ochoa J, et al., Physical examination tests for screening and diagnosis of cervicogenic headache: A systematic review, Manual Therapy (2015), http://dx.doi.org/10.1016/j.math.2015.09.008