INTRODUCTION
Trigger point dry needling (TDN) has become an increasingly common way to address the pain and dysfunction that comes from muscle pain. Myofascial trigger points are excessively irritable points in skeletal muscle that are associated with a painful knot in a taut band (2). Myofascial trigger points (MTrPs) are a common source of musculoskeletal pain in people. MTrPs can be found in a variety of conditions. MTrPs are associated with muscle spasms, increased sensitivity, stiffness, muscle weakness, decreased range of motion, fatigue, and autonomic dysfunction (2,3). Trigger points can be defined as being active or latent and either can produce local or referred pain, hyperalgesia, and allodynia (4). Hyperalgesia and allodynia are defined as a high sensitivity and pain to the touch.
METHODS
The aim of TDN on a MTrPs is to provoke a mechanical tissue stimulation in order to eliminate the MtrP and return the muscle to its normal function (4). Multiple studies have shown that trigger point dry needling immediately increases pain pressure threshold, range of motion, and decreases pain in patients with musculoskeletal disorders (6). The purpose of this systematic analysis (1) is to determine the short-term (0-72 hour), medium-term (1-12 week), and long-term (13-24 week) effectiveness of TDN on MTrPs. 42 studies were included in this meta-analysis after an original review of 102 potential studies that could have been included. The studies included all had to include measurements for pain. The studies were then broken down in to 3 subgroups: TDN versus placebo, TDN versus other therapies, and TDN plus other therapies versus other therapies.
RESULTS
16 of the 42 studies assessed were on neck pain and headaches, 5 on shoulder pain, 5 on knee pain, 3 on lumbar spine pain, 4 on ankle pain, 2 on hip pain, 1 on fibromyalgia, and all others on various musculoskeletal pains.
- Immediately post DN to 72 hours after treatment: low quality evidence, large effect
- 1 to 3 weeks post DN: moderate quality evidence, moderate effect
- 4 to 12 weeks post DN: low quality evidence, large effect
- 13 to 24 weeks post DN: low quality evidence, large effect
DISCUSSION & CONCLUSION
The results of this analysis show that trigger point dry needling produced better results than having no treatment, placebo treatment, sham dry needling, and produces better results than TENS, compression, conventional rehabilitation, massage, stretching, and friction massage. For the time period of immediate to 72 hours post treatment of the application of dry needling, there was a direct correlation between number of sessions of dry needling and trigger points affected creating an increased positive outcome. The best thought at this time as to why dry needling leads to a reduction in pain and improved function is due to an increase in blood flow to the area where the needling was performed, decreased presence of substance P-the bodies pain alerting peptide, and the overloading of the muscle that occurs when the needling creates a muscle twitch, which ultimately improves muscle activation and function similar to that of an intense workout (7,8). At this time the best recommendation for dry needling is 1 session per week to be effective (1).
For the time period of 4-12 weeks post needling, dry needling was again found to be more effective than most or all other therapies performed individually (1). And no specifics are provided for this time frame as to the appropriate number of sessions to be most beneficial, so further evidence is needed. For the time period of 13-24 weeks post TDN, the evidence at this time is extremely limited, so further research must be completed. It was however determined that the sooner a trigger point is treated upon its onset, the longer lasting the results (acute responds faster and longer than chronic) (1).
In summary, low to moderate quality evidence at this time shows a moderate to large effect of trigger point dry needling in reducing overall pain levels and improving muscle function. Further studies of higher quality are needed, but at this time trigger point dry needling is an effective treatment that comes at very little cost in regards to both time and money, and demonstrates nominal negative effects.
TDN is now legal in 36 states to be performed by PTs, the law is silent on PTs performing TDN in 8 states, and is prohibited in 6 states (9). The following infographic best displays the legality by state. TDN is legal to be performed by PTs in the State of Maryland, and Maryland requires the strictest dry needling education and competency requirements of any state in the US (10).
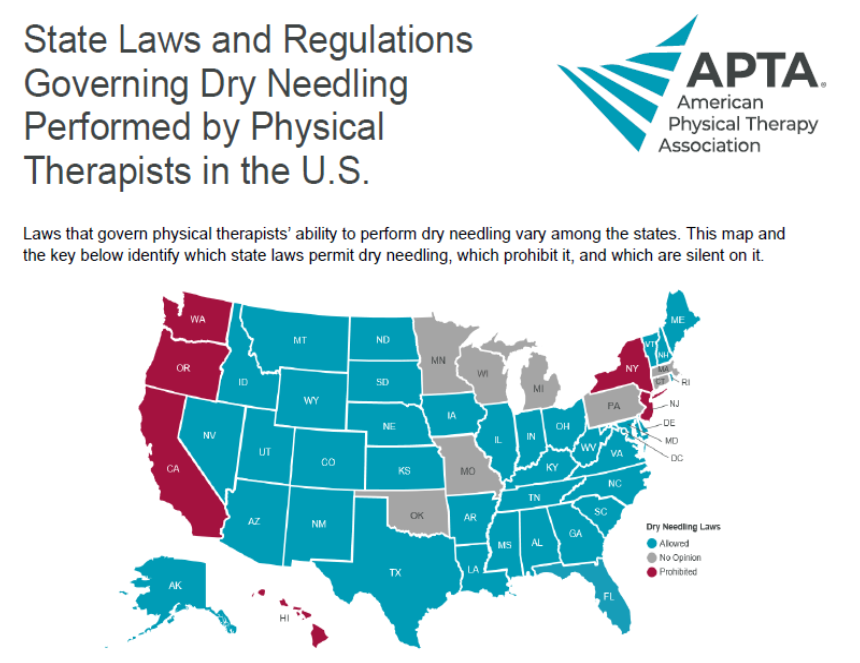
Image courtesy of the American Physical Therapy Association (9)
Physical Therapy First
The clinical team at Physical Therapy First has more physical therapists certified in trigger point dry needling than anyone else in the Greater Baltimore region. Our team of board certified orthopedic clinical specialists provides you with a one-on-one appointment for one hour with a doctor of physical therapy, at any of our 4 greater Baltimore locations.
References
This article is a summary from reference #1, cited below.
1. Sánchez-Infante J, Navarro-Santana MJ, Bravo-Sánchez A, Jiménez-Diaz F, Abián-Vicén F. Is Dry Needling Applied by Physical Therapists Effective for Pain in Musculoskeletal Conditions? A Systematic Review and Meta-Analysis. PTJ: Physical Therapy & Rehabilitation Journal | Physical Therapy, 2021;101:1–15.
2. Donnelly JM, Fernándezd el as Peñas C, Finnegan M, Freeman JL. Travell, Simons & Simons’ Myofascial Pain and Dysfunction: the Trigger Point Manual. 3rd ed. Philadelphia, PA, USA: Wolters Kluwer; 2018.
3. Kamanli A, Kaya A, Ardicoglu O, et al. Comparison of lidocaine injection, botulinum toxin injection, and dry needling to trigger points in myofascial pain syndrome. Rheumatol Int. 2005;25:604–611.
4. Hall ML, Mackie AC, Ribeiro DC. Effects of dry needling trigger point therapy in the shoulder region on patients with upper extremity pain and dysfunction: a systematic review with meta-analysis. Physiotherapy. 2018;104:167–177.
5. Dommerholt J,Mayoral del Moral O, Gröbli C. Trigger point dry needling. J Man Manip Ther. 2006;14:203–201.
6. Gattie E,Cleland JA, Snodgrass S. The effectiveness of trigger point dry needling for musculoskeletal conditions by physical therapists: a systematic review and meta-analysis. J Orthop Sports Phys Ther. 2017;47:133–149.
7. Pecos-Martín D,Montañez-Aguilera FJ,Gallego-Izquierdo T, et al. Effectiveness of dry needling on the lower trapezius in patients with mechanical neck pain: a randomized controlled trial. Arch Phys Med Rehabil. 2015;96:775–781.
8. Ibarra JM, Ge HY,Wang C, et al. Latent myofascial trigger points are associated with an increased antagonistic muscle activity during agonist muscle contraction. J Pain. 2011;12:1282–1288.
9. https://www.apta.org/patient-care/interventions/dry-needling/laws-by-state
10. https://health1.maryland.gov/bphte/Pages/dryneedling.aspx
