by Jeslin Thomas
It’s not as tricky as you may think. If you are curious or have been diagnosed with one of these, the therapists at PT First can help you out!
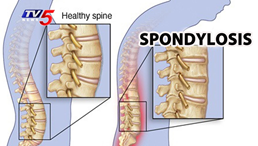
Spondylosis: refers to when you have degenerative osteoarthritis (OA) of the spine- this essentially means that the space between your vertebrae narrows as the protective cartilage that cushions the ends of the vertebrae wears down with age. With time, you may notice you have more of a flexed (forward bending) posture. Individuals suffering from this may experience lower back pain, leg pain, and/or numbness when standing or walking; symptoms may only seem to improve with sitting or lying down1.
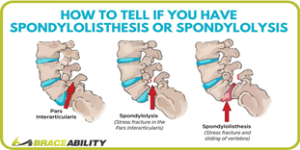
Spondylolysis: refers to a stress fracture defect in the pars interarticularis of the vertebrae (commonly found in the L4/L5 region). This is usually caused by repetitive stress or trauma at the Lumbar spine from strenuous activities involving excessive twisting/rotating or back bending (ex: gymnastics, dancing, wrestling, and football.). Symptoms may or may not be present initially, but as the injury progresses, these individuals may complain of pain as they bend backward or pain with general activities2.
Spondylolisthesis: often refers to the progression of a spondylosis injury, but it may also be congenital or idiopathic in nature. Spondylolisthesis is defined as the displacement of one vertebra over the vertebral body below it (commonly known as a “step off” or “slip” at the L5/S1 level); individuals may even notice the presence of a bump by the area of the slippage. There are 5 different grades of this slippage, and it’s defined by the extent to which the vertebral body has slipped:
Grade I: O-25% Grade III: 50-75% Grade V: > 100%
Grade II: 25-50% Grade IV: 75-100%
Individuals with this may complain of localized pain that may come and go with certain activities, and this may be the most notable when bending backward or forward at the affected segment. They may experience radicular pain down to one or both legs as the vertebrae slides and causes compression of the nerve root below, tense hamstrings, loss of bowel/bladder (rare), and difficulty with balance or walking.
What can we do?
First, you can consult with your Doctor to obtain an MRI, CT, Bone scan, or X-ray to confirm the diagnosis and determine the extent of the injury. Treatments can involve both operative (surgical) or nonoperative/conservative management (Physical Therapy, NSAIDs/analgesics, and bracing). Generally, surgical interventions are reserved for those with significant symptoms or failure of conservative treatments.
With spondylosis, conservative management involving aerobic exercises such as biking and general strengthening and stretching of your whole body has been correlated to greater quality of life among adults with lumbar osteoarthritis 3. In addition, maintaining good posture throughout and maintaining our postural muscle strength can help to decrease pain and promote proper muscle length-tension relationships.
With spondylolysis, as with any fracture, your body will need time to heal. This means 4-8 weeks (or longer) of rest from high impact activities such as sports and lifting heavy items. Your Doctor may also recommend pain medications such as NSAIDs or steroids to help reduce pain and inflammation. During this time, Physical Therapy may be recommended and can help with facilitating the healing process, reduce pain, strengthen and stabilize specific muscles, and help you navigate through your everyday activities.
In addition, with both spondylolysis and spondylolisthesis, studies have shown that specific strengthening of the deep multifidus and transversus abdominis can be beneficial for spinal instability that commonly occurs 3,4. Overall, exercises to promote the full spinal range of motion and lumbar strengthening exercises have been proven to be a successful treatment option for decreasing pain and functional limitations 2,4,5. At PT First, our therapists have treated multiple patients with success when using this evidence-based method. If you have any questions, don’t hesitate to ask any of our licensed therapists!
References
Middleton, Kimberley, and David E. Fish. “Lumbar Spondylosis: Clinical Presentation and Treatment Approaches.” Current Reviews in Musculoskeletal Medicine 2, no. 2 (March 25, 2009): 94–104.
Garet M, Reiman MP, Mathers J, Sylvain J. Nonoperative treatment in lumbar spondylolysis and spondylolisthesis: a systematic review. Sports Health. 2013;5(3):225-232. doi:10.1177/1941738113480936
VIEIRA, S., et al, Abdominal muscle strength is related to quality of life among older adults with lumbar osteoarthritis. Journal of bodywork and movement therapies, 2015. (level of evidence 2A)
Kalichman L, Hunter DJ. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J. 2008;17(3):327-335. doi:10.1007/s00586-007-0543-3
Back Pain: Spondylosis, Spondylolysis, and Spondylolisthesis. SPARCC Sports Medicine – Tucson AZ. https://sparcctucson.com/2019/03/21/back-pain-spondylosis-spondylolysis-and-spondylolisthesis/. Published October 23, 2019. Accessed August 2, 2020.
Images:
https://www.braceability.com/blogs/articles/lumbar-spondylolisthesis-vs-spondylolysis
www.youtube.com/watch?v=3SoNJ5ELR6Y
