INTRO
Headaches are a common complaint for many people, and most assume that it is just normal part of life. Some may experience headaches multiple times per week or even daily. Patients often report that headache medication may help reduce the severity of the symptoms, but does not eliminate them entirely or stop them from coming back. If this is true for you, it may be a sign that your headaches are related to dysfunction in your neck. Both tension headache and the various forms of migraine headaches will likely have a musculoskeletal component.
CERVICOGENIC HEADACHE
The term “cervicogenic headache” indicates that although pain is felt in the head, the root cause of the symptoms related to the neck (cervical spine). Common root causes of head and facial pain include:
– Altered cervical spine alignment
– Forward head posture
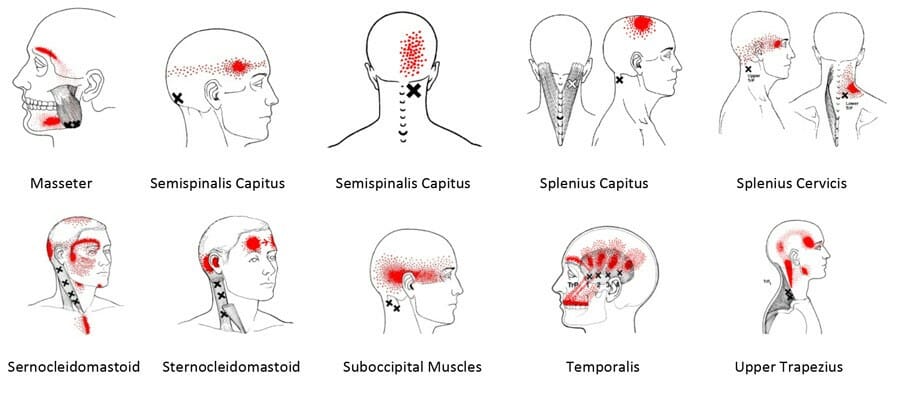
– Muscle tightness or trigger points in the following muscles (see figure above)
– Upper Trapezius
– Suboccipitals
– Sternocleidomastoid
– Splenius capitus and Splenius cervicis
– Shallow breathing pattern using the neck muscles
– Jaw clenching or grinding
STRESS
Now, what about those who just attribute their headaches to work-life stress? While it may be true that the headache feels worse during times of stress, it could be related to some of the root causes listed above. During a stressful meeting, do you resort to a shallow breathing pattern and overwork the neck muscles? Or, while concentrating on work, are you holding tension in your jaw or facial muscles and clenching? Each of these, over time and with repetition, has the potential to create trigger points in the neck muscles that can lead to referred pain in the head and face.
Physical Therapy for headaches begins with an exam of your neck alignment, posture, muscle strength, and breathing pattern. Treatment involves postural correction and neck strengthening, releasing trigger points, correcting breathing patterns, and improving postural and muscle awareness. If you feel that these factors could be a cause of your headaches, Physical Therapy First can help identify and treat these issues.
RED FLAGS
There are times when the headache is more than “cervicogenic,” and the following red flags from The Amercian Migraine Foundation indicate the need for medical attention:
- Thunderclap Headache: very severe headache that reaches its maximum severity immediately (within a couple of minutes). Thunderclap headaches require emergent medical evaluation.
- Positional Headache: headache that substantially changes in intensity in association with changes in position – e.g. standing from lying or vice-versa.
- Headaches Initiated by Exertion: headache starting while coughing, sneezing, and/or straining.
- New Headaches: especially if older than 50 years of age, or if there are medical conditions that make worrisome headaches more likely (e.g. cancer, blood clotting disorder).
- Substantial Change in Headache Pattern
- Constant Headache Always in the Same Location of the Head
- Worrisome Neurologic Symptoms: about 1/3 of people with migraine have neurologic symptoms (“migraine aura”) that typically precede onset of a migraine headache. Commonly, aura symptoms consist of slowly spreading visual symptoms sometimes accompanied by tingling of the face and upper extremity. These symptoms resolve within 60 minutes. If these symptoms have immediate onset (as opposed to a slow progression of symptoms), last longer than 60 minutes, or do not completely resolve, medical attention is required. Medical attention is also required if other symptoms are present, such as weakness of one side of the body, change in level of consciousness, significant difficulty walking, or other symptoms that worry you.
- Headache that never goes away
- Systemic symptoms: including fever, chills, weight loss, night sweats
SOURCES
(1)Travell JG, Simons DG. Myofascial Pain and Dysfunction, The Trigger Point Manual, Vol. 1. Baltimore. Williams and Wilkins. 1993
(2) American Migraine Foundation
