Reviewed by Jerome Thomas, SPT, Tyler Tice, PT, DPT, OCS, ATC
Patellofemoral pain syndrome (PFPS) is a chronic musculoskeletal condition characterized by persistent anterior knee pain. This condition is sometimes referred to as “runner’s knee” because it is common in individuals who participate in sports or recreational activities. However, patellofemoral pain syndrome can also occur in nonathletes as the increased pain levels and stiffness can make it difficult to climb up stairs, kneel down, and other activities of daily living.
Often times, a multimodal approach is utilized to treat individuals with PFPS. However, there is very little evidence to support the idea that the current multimodal approach for treatment of PFPS leads to successful clinical outcomes. A research study by Brown et al. on patients with PFPS, showed that only 46% of patients’ knees were pain-free at discharge. Based on the failures of the current multimodal treatment approach, there has been a strong recommendation from the International Patellofemoral Pain Research Retreats to clinically subgroup patients with PFPS and deliver targeted treatments. This prospective crossover intervention categorized patients with PFPS into 3 subgroups to assess whether targeted treatments would show clinical benefits over a multimodal approach.
The participants for this study were between the ages of 18 and 40, attending a physical therapy outpatient clinic at a university hospital with a clinical diagnosis of PFP. Various assessment tools were utilized to categorize the patients with PFPS: quadriceps and hip abductor muscle strength in the form of manual muscle tests, patella glide test, quadriceps length, gastrocnemius length, and the foot posture index. Based on these PFPS criteria, the participants were classified into 1 of 3 subgroups: strong, weak and tight, or weak and pronated feet.
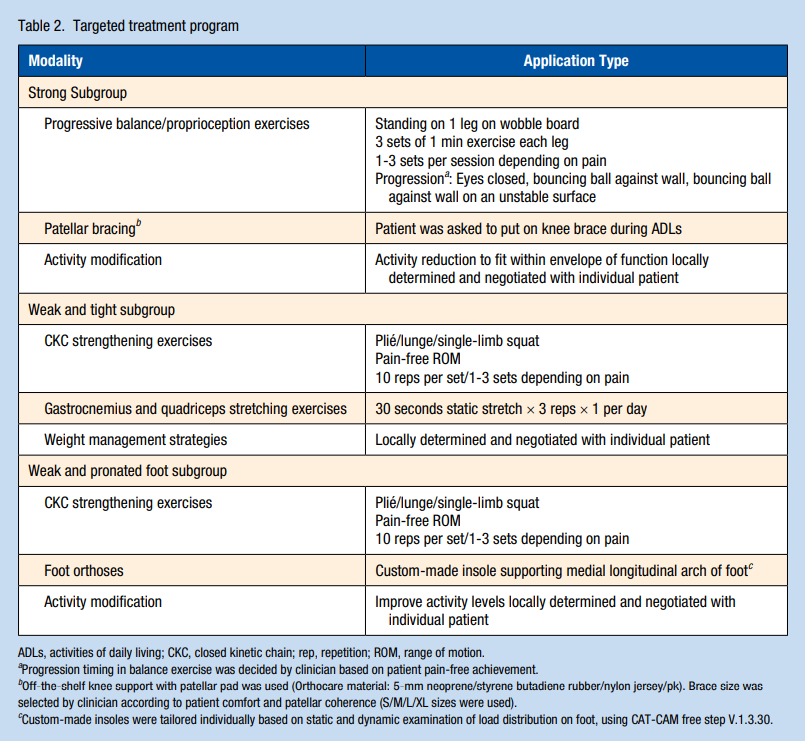
All 61 patients in this crossover intervention study were given 6 weeks of multimodal treatment. The multimodal treatment included thermotherapy (heat application), transcutaneous electrical neural stimulation (TENS), stretching, as well as hip and knee strengthening. 21 patients responded positively to this treatment approach but 40 patients were non-responders to this approach. The 40 PFPS non-responders were then given an additional 6 weeks of targeted treatment based upon one of the three subgroups they were classified within. The intervention program for the “strong” subgroup was targeted at improving neuromuscular control and coordination ability using proprioceptive exercises. In the “weak and tight” subgroup, the exercise program consisted of closed kinetic chain (CKC) muscle strengthening and stretching and weight management advice. Lastly, the “weak and pronated foot” subgroup had an intervention program that included CKC strengthening exercises and foot orthoses.
Pain during activity measured using a visual analog scale (VAS) was the primary outcome measure of this study. The perception of recovery scale (PRS) was also utilized where patients rated themselves from “worse than ever” to “completely recovered” on a 7-point scale. The results of the study showed that 72.5% (29 patients) of the 40 PFPS non-responders demonstrated recovery after targeted treatment approaches. Recovery was measured through improved pain intensity (VAS) scores at rest and during activity, as well as significantly improved PRS scores. The findings of this intervention study suggest that targeted interventions based on subgroups provide a more effective treatment strategy for patients with PFPS.
Clinical Application:
Patients with PFPS who do not respond positively to the current multimodal treatment approach may benefit from a more targeted treatment. Targeted subgroups used to classify PFPS patients as “strong,” “weak and tight,” or “weak and pronated foot” provide a blueprint for targeted interventions that can improve clinical outcomes. Below is a graphic that outlines the targeted interventions for each subgroup:
References:
Yosmaoğlu HB, Selfe J, Sonmezer E, et al. Targeted Treatment Protocol in Patellofemoral Pain: Does Treatment Designed According to Subgroups Improve Clinical Outcomes in Patients Unresponsive to Multimodal Treatment?. Sports Health. 2020;12(2):170-180. doi:10.1177/1941738119883272
Brown J. Physiotherapists knowledge of patellofemoral pain syndrome. Br J Ther Rehabil. 2000;7:346-353.
